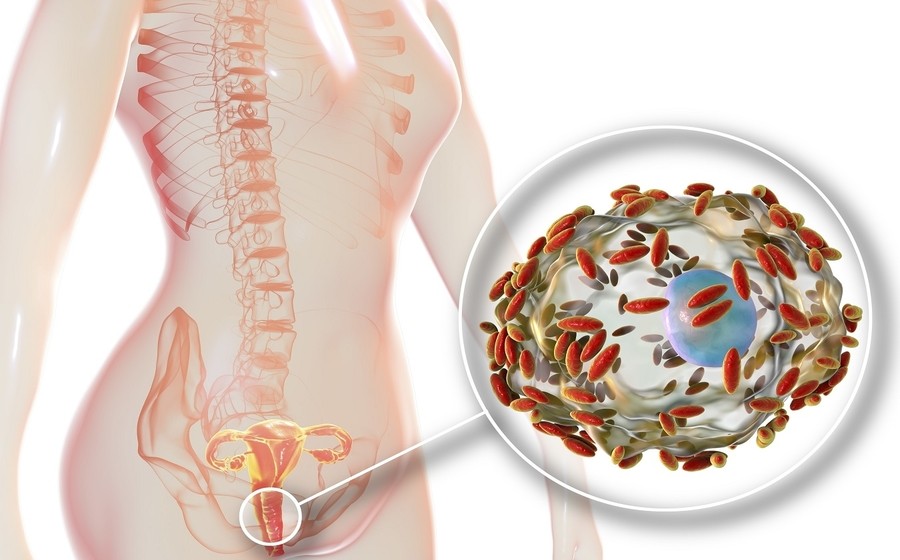
In the last decade, many clinical trials have been conducted to assess the effects of probiotics in the prevention and treatment of a broad range of disorders, and the scientific interest in this field is growing. The rationale of using oral probiotics in the treatment of gynaecological conditions is related to the ability of these microorganisms to survive through the gastrointestinal system and to ascend to the vaginal tract after their excretion from the rectum; whereas vaginal administration allows a direct and targeted colonization action of the probiotics for restoring healthy vaginal microbiota.1
Probiotics in Non-Pregnant Women
Vaginal infections represent one of the most common reason for gynaecological consultation.
Bacterial vaginosis is the most common type of vaginal infection among women of reproductive age and accounted for at least one-third of all vulvovaginal infections. Bacterial vaginosis (BV) is an ecological imbalance of the vaginal microbiota affecting mostly women of reproductive age group. There is a decrease in vaginal acidity and in the concentration of lactobacilli accompanied by an increase of a 100-fold or more in the concentration of other micro-organisms. Lactic acid produced by the normal flora, which is Lactobacillus spp. causes hydrogen peroxide (H2O2) production, which is attributed to the acidic milieu of the vagina. This provides a local defense mechanism by inhibiting the growth of other organisms. Change in the normal vaginal flora causes change in pH simultaneously, which allows a variety of anaerobes and facultative bacteria to overgrow and cause chronic infection as well as abnormal vaginal discharge. BV is a clinical condition characterized by a thin, gray/off-white, homogenous, malodorous adherent vaginal discharge which is more noticeable after intercourse and menses, having pH > 4.5. Fishy odor is noticed on addition of 10% potassium hydroxide to the vaginal fluid (whiff test), and the presence of clue cells, a few or no lactobacilli, and small number (<1/hpf) of polymorphonuclear leucocytes (PMNs) are also the characteristic features of BV.
A trial was conducted on 120 female adults who were suffering from bacterial vaginosis and were treated with 120 million CFU/g of Bacillus coagulans SNZ 1969 tablet co-administered with T. Metronidazole 400 mg tablet thrice a day for 21 days. Significant reduction in symptoms and scoring was observed with the Bacillus coagulans SNZ 1969 +T. Metronidazole Vs plain T. Metronidazole.2
In another trial with 100 adult females suffering from vaginitis were given single tablet of Bacillus coagulans SNZ 1969 twice daily for 3 days and then once daily for the next 4 days. About 92% patients had complete relief from symptoms with the treatment.3
Another vaginal disorder which is common among young female population is Leucorrhea which might not be a major issue but it’s best to be resolved as soon as possible. In Leucorrhea, there is thick, whitish or yellowish vaginal discharge mainly due to estrogen imbalance but can increase during vaginal infection. Bacillus coagulans SNZ 1969 has been proven to be beneficial when administered in such cases and can lead to more than 80% symptomatic relief. An Indian trial was conducted with 25 females between the age of 18-40 years and it was found out that when these females were administered with 1 tablet of Sporlac(Bacillus coagulans SNZ 1969) in vagina for a week, 64% showed complete symptomatic relief, 20% showed moderate relief and 16% experienced no change in symptoms.4
In another multi-centre clinical assessment of125 females between the age group of 18-50 suffering from symptoms of Leucorrhea, were treated with Myconip (Bacillus coagulans SNZ 1969) 1 tablet twice a day for 7 days. The results of the trial showed complete relief in 101 patients i.e. 82% overall improvement.5
Role of probiotics as per International guidelines for the treatment of vulvovaginal infections6